Le Sepsis
Le sepsis : une urgence médicale fréquente, coûteuse et difficile à diagnostiquer

49 millions de cas et 11 millions de décès en 2017

Coût des traitements et du diagnostic: 5.1Mds$ en 2024
Croissance estimée de 6-8%/an jusqu’en 2030

Un impact économique lourd pour les systèmes de santé: 52Mds$ en 2021 aux USA
Besoin d’un marqueur de diagnostic précoce et d’évaluation de la sévérité du sepsis pour guider la prise de décision du clinicien
Il est essentiel de développer un marqueur délocalisé efficace pour évaluer rapidement la sévérité de l’état clinique des patients dès leur admission en réanimation ou aux services d’urgences.
Pr Sami Hraiech
Médecine Intensive, Réanimation – APHM
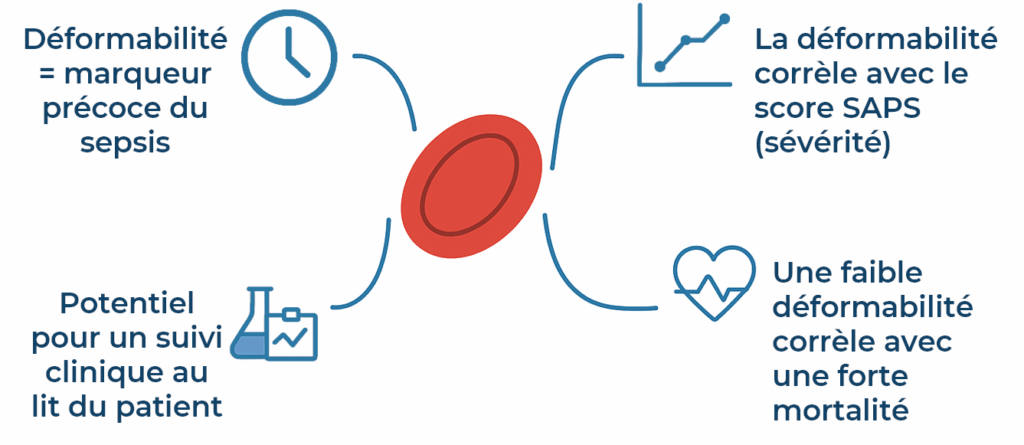
La déformabilité des globules rouges, un marqueur de pronostic précoce et de sévérité du sepsis
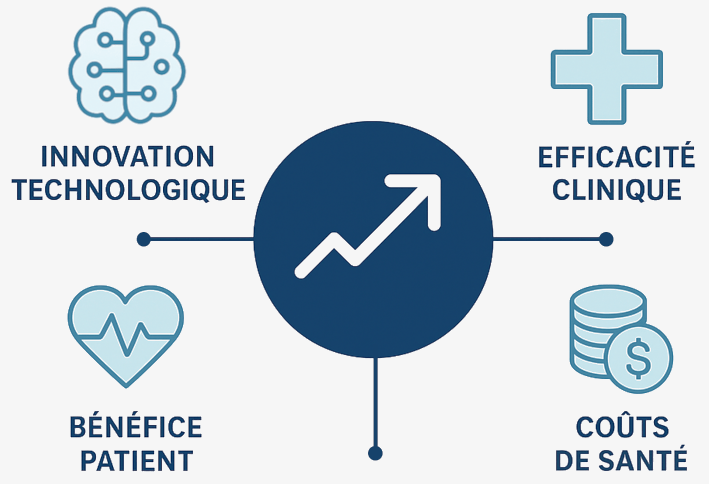
Notre proposition de valeur
Avec la technologie DYNARED, nous ambitionnons de fournir au clinicien un marqueur performant et rapide pour guider sa prise de décision, augmenter les chances de survie du patient tout en optimisant les coûts de santé publique
- Katia Donadello et al. Reduced red blood cell deformability over time is associated with a poor outcome on septic patients, Microvascular Research 2015, DOI: 10.1016/j.mvr.2015.05.001
- A.G. Moutzouri et al. Red blood cell deformability in patients with sepsis: A marker for prognosis and monitoring of severity, Clin. Hemorheol. Microcirc. (2007), PMID: 17502699


